Understanding Hypertension: Misdiagnosis and Effective Management
Written on
Chapter 1: The Challenge of Hypertension Diagnosis
Blood pressure assessments by healthcare professionals can often be misleading. The inaccuracies stem not from the doctors themselves but rather from the complexities of human physiology and hemodynamics. Fortunately, there are straightforward strategies you can employ to mitigate these inaccuracies.
The significance of this issue cannot be understated. Misdiagnoses can lead to inappropriate medication use or, conversely, neglecting necessary treatments.
What should you do next? The rallying cry is clear: “Know your numbers!” This phrase encapsulates the essence of the WHO’s 2024 Hypertension Day theme. In this article, I will guide you on how to effectively apply this principle.
The Battle Against Blood Pressure Mismanagement
Most healthcare providers have been queried multiple times about alternatives to pharmacological treatments for hypertension. The most crucial alternative I could suggest is simply to "know your numbers." This statement may seem vague now, but its importance will become clear.
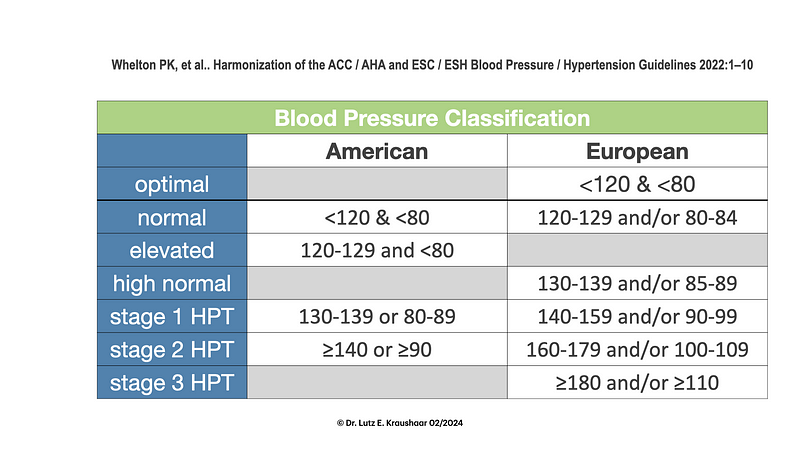
Doctors often rely on specific numerical values to determine if you have hypertension. However, there exists a remarkable level of inaccuracy in these measurements. Understanding blood pressure involves more than just noting systolic and diastolic values (SBP and DBP).
There are numerous treatments available—11 distinct classes of antihypertensive medications—yet they do not uniformly benefit all patients. This variability indicates that hypertension can manifest in various forms, complicating its treatment.
As a researcher in hemodynamics for two decades, I will demonstrate how you can assume a more proactive role in managing, preventing, and potentially reversing hypertension for yourself or your loved ones.
Key Takeaways:
- Assess the reliability of your blood pressure readings (the results may surprise you).
- Explore potential causes and pathways related to elevated blood pressure.
- Understand the N-of-1 method to identify what works best for you.
Understanding Blood Pressure Variability
When I first meet with clients and ask about their blood pressure, I often hear something like, “It’s usually around 120/80 at home, but higher at the doctor’s office.” This common realization highlights a crucial fact: blood pressure is inherently variable.
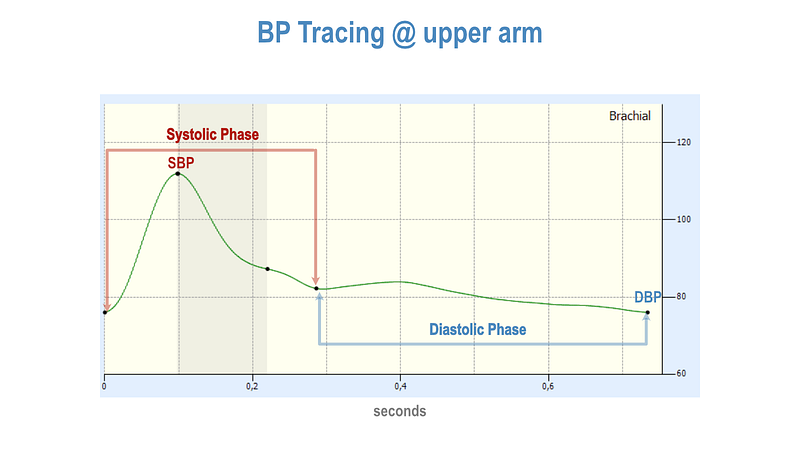
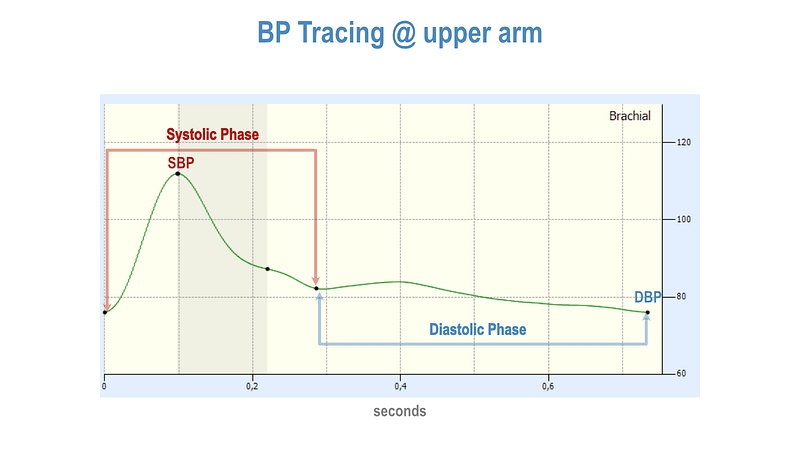
This variability can occur from heartbeat to heartbeat, and even within a single heartbeat, as illustrated below. It can fluctuate from moment to moment, influenced by factors like physical relaxation or emotional distress. Blood pressure also shows daily and seasonal variations.
Section 1.1: Questioning Your Diagnosis
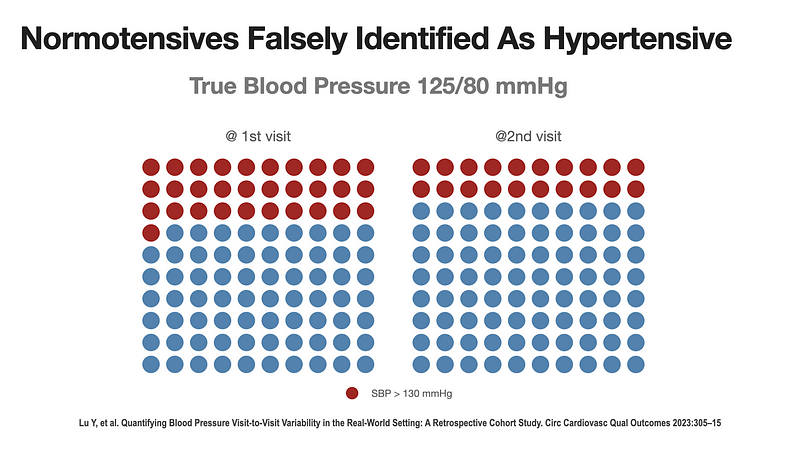
Researchers from Yale University’s Center for Outcomes Research and Evaluation analyzed 7.7 million blood pressure readings from over 537,000 adults. They focused on variations in readings taken no longer than 90 days apart. This timeframe is ideal because it typically prevents chronic factors from skewing results.
Remarkably, in 95% of cases, the average systolic blood pressure varied by 21.2 mmHg between visits. This wide margin means it's possible to go from normal blood pressure at one appointment to stage-2 hypertension at the next.
This comprehensive study provides valuable insights into how often blood pressure readings can mislead. To illustrate, let’s assume you and 99 others with a “true” systolic pressure of 125 mmHg visit a doctor. About 30% of you might receive a reading above 130 mmHg, suggesting potential hypertension, despite having normal blood pressure.
A follow-up visit within three months would likely show that only 20 out of those 30 still register above that threshold, resulting in a significant number of unnecessary consultations and diagnoses.
Section 1.2: The Reality of Blood Pressure Measurement
How often do healthcare providers follow proper blood pressure measurement protocols, such as taking three readings one minute apart?
The American Heart Association (AHA) has guidelines similar to those in Europe, but they often overlook the recommended practices.
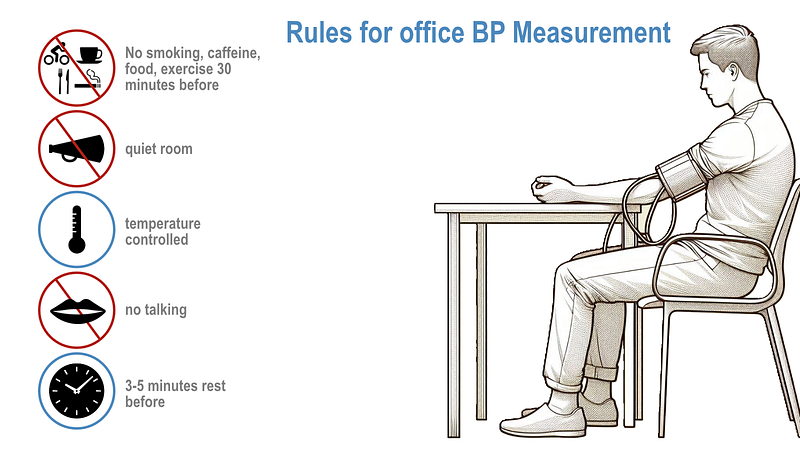
In practice, patients are frequently rushed through appointments without adequate preparation, which can lead to erroneous readings.
Chapter 2: Home Blood Pressure Monitoring
To counteract these issues, many health organizations now advocate for home blood pressure monitoring (HBPM) as a superior alternative to office measurements.
Several guidelines endorse self-measured blood pressure monitoring as essential for diagnosing and managing hypertension. HBPM can reveal the white-coat effect (where patients exhibit elevated blood pressure due to anxiety during medical visits) and masked hypertension (where patients remain undiagnosed).
The U.S. Preventive Services Task Force has recommended HBPM as an alternative when ambulatory blood pressure measurement (ABPM) is impractical. However, ABPM can be uncomfortable for patients, making it less desirable.
To ensure accurate home measurements, consider the following:
Equipment: Choose validated upper-arm devices over wrist monitors for better accuracy.
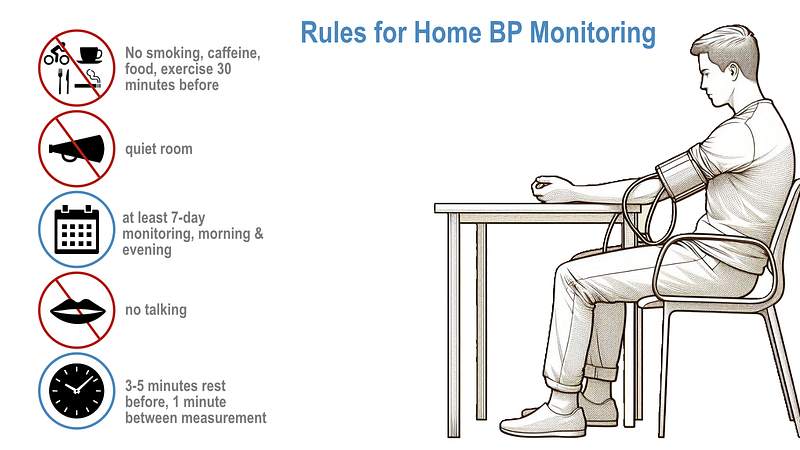
Procedure: Follow established procedures for consistent readings, such as measuring at the same time each day.
Monitoring Schedule: For the most reliable results, measure blood pressure at similar times, ideally in the morning and evening.
The Hidden Insights in Your Blood Pressure Values
Understanding the significance of systolic and diastolic numbers is just the beginning. The difference between these two values is known as pulse pressure (PP), and mean arterial pressure (MAP) can also provide valuable insights.
MAP correlates better with certain health risks than either SBP or DBP, making it a useful benchmark for tracking your response to various interventions.
The Mechanisms of Circulation
The circulatory system operates under certain physical laws, where flow, pressure, and resistance are interlinked. Factors like cardiac output and resistance influence MAP and DBP, while arterial compliance and stroke volume affect PP and SBP.
As we age, arterial compliance tends to decrease, leading to increased PP and SBP. Yet, lifestyle choices significantly impact arterial health.
The Practical Takeaways: Risk Markers and Causes
Different age groups experience varying risk indicators: for adults under 50, elevated DBP is a key concern; above 60, PP becomes more relevant; while between 50 and 60, SBP is critical.
The strategies for managing hypertension include targeting interventions based on identified risk factors and focusing on lifestyle changes that can improve compliance and reduce resistance.
The N-of-1 Method: Personalizing Your Approach
Research suggests that tailoring treatment to individuals can lead to better blood pressure control. This principle is the essence of the N-of-1 method, which emphasizes a personalized approach to lifestyle modifications.
With the N-of-1 method, you can test different interventions and observe their effects on your blood pressure, enabling a more customized approach to health management.
To further explore this topic, consider watching the following informative videos:
The first video titled "High Blood Pressure (Hypertension): Symptoms & Ways to Lower It" from Mass General Brigham provides insights into understanding hypertension better.
The second video, "Why Me? Getting a High Blood Pressure Diagnosis and What You Can Do About It," delves into the implications of a hypertension diagnosis and actionable steps to take.
Conclusion: Embracing the "Know Your Numbers" Philosophy
In conclusion, understanding your blood pressure—its variations, the potential for misdiagnosis, and how to measure it accurately—is crucial. The World Health Organization echoes this sentiment with their motto for World Hypertension Day: “Measure Your Blood Pressure Accurately, Control It, Live Longer.”